First cardiac bioimplants for the treatment of patients with myocardial infarction using umbilical cord stem cells

- The results of a pioneering study support the safety of the bioimplants called PeriCord, made from stem cells of the umbilical cord and pericardium from a tissue donor, which aid in the regeneration and revascularisation of the affected area.
- The study has monitored 7 interventions of this pioneering tissue engineering surgery over three years, noting excellent biocompatibility and no rejection in patients.
- The therapy has been developed by the research group ICREC (Heart Failure and Cardiac Regeneration) at Germans Trias i Pujol Research Institute (IGTP) and Banc de Sang i Teixits (BST).
- PeriCord has anti-inflammatory properties and opens the door to creating other drugs for conditions beyond the heart.
The promising results obtained in a clinical trial with a pioneering advanced therapy drug named PeriCord, which aims to repair the heart of patients who have suffered a heart attack, confirm the feasibility of new therapies based on the application of stem cells and tissue engineering to promote the regeneration of damaged tissues.
This new medicine, derived from umbilical cord and pericardium stem cells from tissue donors, is a world-first tissue engineering product (a type of advanced therapy combining cells and tissues optimised in the laboratory). The drug is applied in patients undergoing coronary bypass, utilising the procedure to repair the scar in the heart area affected by the infarction, which has lost the ability to beat when blood flow stopped.
The first intervention of this new therapy was almost 4 years ago, resulting from a collaboration between the ICREC Group (Heart Failure and Cardiac Regeneration) at Germans Trias i Pujol Research Institute (IGTP) and Banc de Sang i Teixits (BST). Following its success, a study was initiated to demonstrate its clinical safety. The study included 12 coronary bypass candidates, 7 treated with bioimplants and 5 without, to compare the outcomes.

Dr Antoni Bayés, ICREC researcher and first author of the article: "This pioneering human clinical trial comes after many years of research in tissue engineering, representing a very innovative and hopeful treatment for patients with a heart scar resulting from a heart attack", referring to PeriCord.
While the current study aimed to demonstrate the safety of this new drug in the context of myocardial infarction, its positive outcomes have shown that PeriCord possesses other exceptional properties. It has proven to be a medicine with excellent biocompatibility, drastically minimising the risk of rejection and ensuring perfect tolerance by the body. Additionally, it has anti-inflammatory properties, paving the way for broader applications in pathologies involving inflammation. "Its potential could be much wider; we believe it can be a valuable tool for modulating inflammatory processes", explains Dr Sergi Querol, head of the Cellular and Advanced Therapies Service at BST.
Severe but stable patients
The patients included in the therapy are individuals who have suffered a heart attack and have reduced quality and life expectancy. The bypass ensures blood circulation in the area, and the bioimplant goes a step further to stimulate the scar, initiating cellular mechanisms involved in tissue repair.
"Voluntarily provided substances of human origin are used, both in terms of multi-tissue donor pericardial tissue and mesenchymal stem cells from umbilical cord donors at the birth of a baby", explains Querol. It is very gratifying to think that "thanks to this and the donors, we provide a new therapeutic tool that can improve a patient's quality of life", he adds.
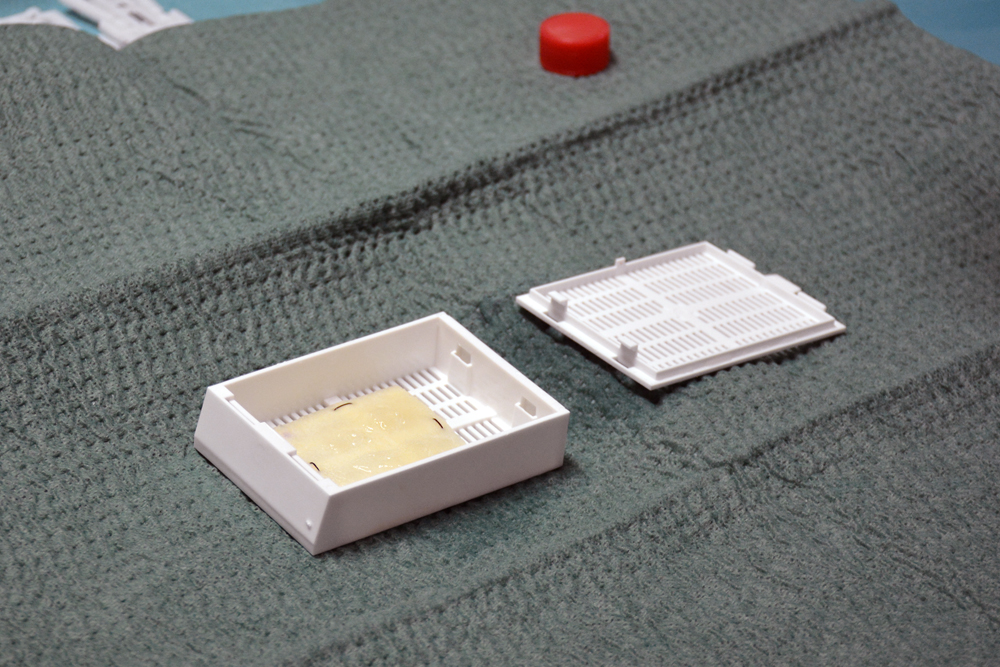
PeriCord consists of a membrane that comes from the pericardium of a tissue donor, which BST has decellularised and lyophilised. It has then been recellularised with these umbilical cord stem cells.
Once in the operating theatre, surgeons attach the laboratory-generated bioimplant to the affected area of the patient's heart. After a year, the implanted tissue adheres and adapts perfectly to the structure of the heart, covering the scar left by the heart attack.
Reference
Bayes-Genis A, Gastelurrutia P, Monguió-Tortajada M, Cámara ML, Prat-Vidal C, Cediel G, Rodríguez-Gómez L, Teis A, Revuelta-López E, Ferrer-Curriu G, Roura S, Gálvez-Montón C, Bisbal F, Vives J, Vilarrodona A, Muñoz-Guijosa C, Querol S. Implantation of a double allogeneic human engineered tissue graft on damaged heart: insights from the PERISCOPE phase I clinical trial. eBioMedicine. 2024 Mar 14;102:105060. DOI: 10.1016/j.ebiom.2024.105060.
